The Pancreas
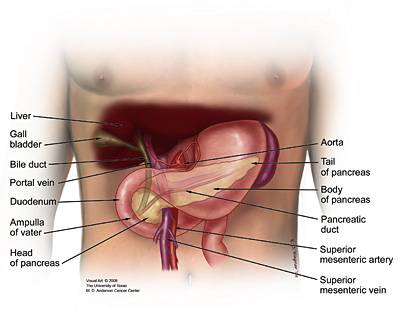
The pancreas is a gland in the abdomen. It’s about six inches long, shaped like a flat pear and surrounded by the stomach, small intestine, liver, spleen and gallbladder. The pancreas is both an exocrine gland and endocrine gland, and it has two main functions: digestion and blood sugar regulation.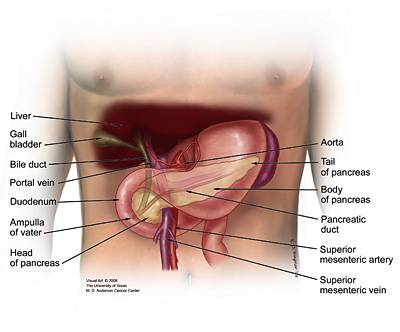
The main pancreatic duct connects with the common bile duct, which carries bile from the gallbladder. Together, they connect with the duodenum at a point called the ampulla of Vater. This is where bile and pancreatic enzymes enter the duodenum to help with the digestion of fats, carbohydrates and proteins.
Pancreatic Cancer
Pancreatic cancer begins when abnormal cells within the pancreas grow out of control and form a tumor. These cells could be either exocrine or endocrine.More than 95 percent of pancreatic cancers are classified as exocrine tumors. These tumors start in the exocrine cells that make pancreatic enzymes that help in digestion. Within this category, the vast majority of tumors are adenocarcinomas.
Pancreatic neuroendocrine tumors (pancreatic NETs or PNETs) account for less than 5 percent of all pancreatic tumors. They may be benign or malignant and tend to grow slower than exocrine tumors.
Risk Factors for Pancreatic Cancer
The exact causes of pancreatic cancer are not yet well understood. However, research studies have identified certain risk factors that may increase the likelihood that an individual will develop pancreatic cancer.- Smoking: Smoking may cause about 20 to 30 percent of all exocrine pancreatic cancer cases. People who smoke cigarettes are two times more likely to develop pancreatic cancer than people who have never smoked.
- Obesity: Obese people have a 20 percent increased risk of developing pancreatic cancer when compared with people who are of normal weight. The risk is even higher in people who are obese during early adulthood. People with excessive abdominal fat may have an increased risk independent of general obesity.
- Race (Ethnicity): African Americans have a higher incidence of pancreatic cancer when compared with individuals of Asian, Hispanic or Caucasian descent. There is also a higher incidence of pancreatic cancer among Ashkenazi Jews.
- Age: The chances of developing pancreatic cancer increases with age. Most people diagnosed with pancreatic cancer are over the age of 60.
- Diet: Although the link between diet and the development of pancreatic cancer is still unclear, a diet high in red and processed meats is thought to increase the risk of developing pancreatic cancer. A diet high in fruits and vegetables may decrease the risk.
Symptoms of Pancreatic Cancer
Pancreatic cancer may cause only vague, unexplained symptoms. If you are experiencing one or more of the symptoms below, we urge you to speak to your doctor immediately and reference pancreatic cancer.Pancreatic Cancer Diagnosis
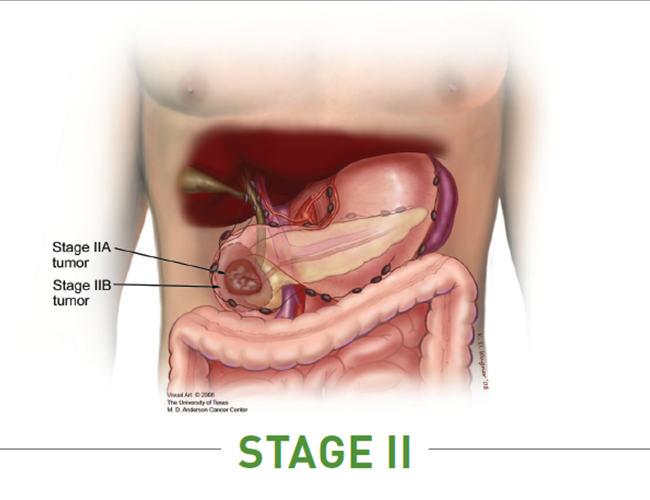
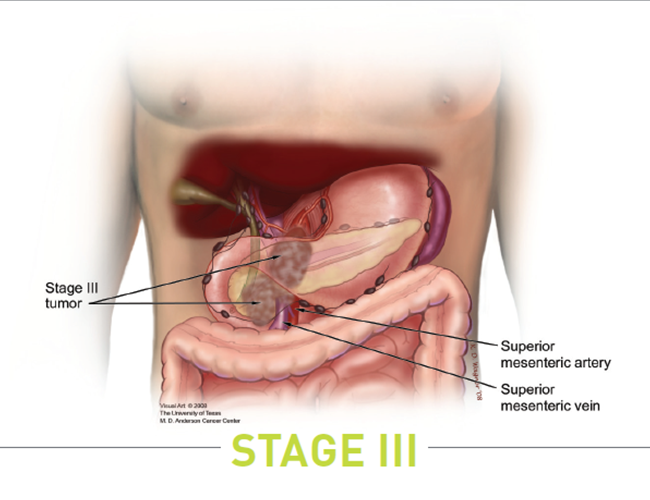
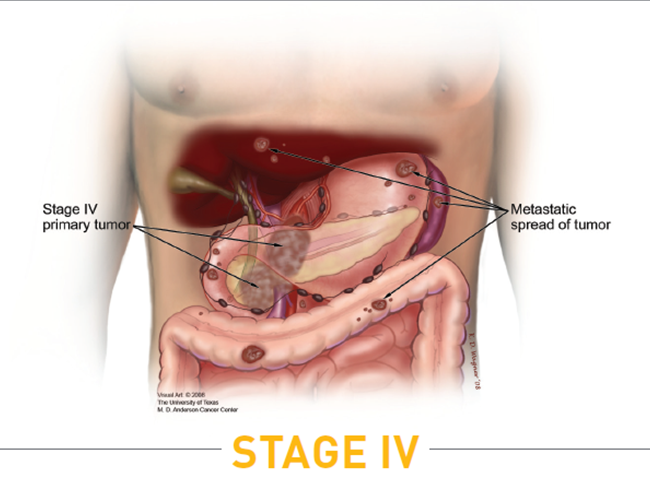
Staging is the process doctors use to determine the extent of the cancer in the body. After a pancreatic cancer diagnosis has been made, additional imaging tests and surgery may be required to accurately determine the stage. Learn more about the staging of pancreatic cancer.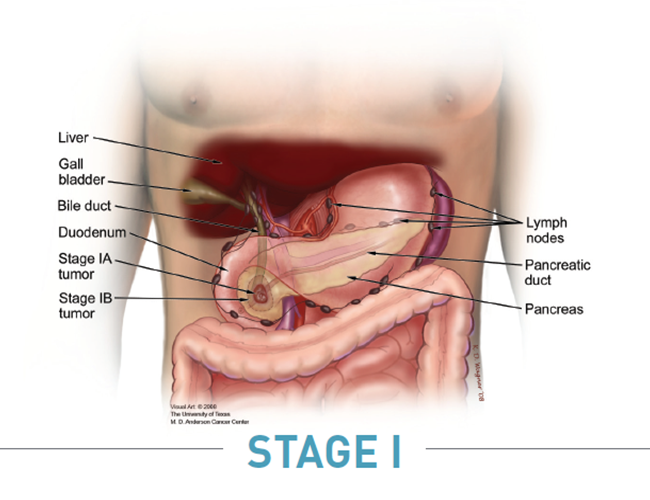
Treatments for Pancreatic Cancer
You are your own best advocate. We strongly recommend that you discuss your treatment goals with your healthcare team and know all your options at every stage of your disease.We maintain the most comprehensive database of available pancreatic cancer clinical trials in the United States. Our Patient Central Associates are available to perform a personalized search for you, or you can start your own search through our Clinical Trial Finder.
Pancreatic Cancer Support
No one should have to face pancreatic cancer alone. We’re here for you. If you or someone you know has been diagnosed with pancreatic cancer, please call a Patient Central Associate toll-free at 877-272-6226 (Monday to Friday, 7 a.m. to 5 p.m. PT) or email patientcentral@pancan.org to speak with a knowledgeable, compassionate associate. Visit our Patient and Caregiver Services for more pancreatic cancer resources.
Information provided by the Pancreatic Cancer Action Network, Inc. (“PanCAN”) is not a substitute for medical advice, diagnosis, treatment or other health care services. PanCAN may provide information to you about physicians, products, services, clinical trials or treatments related to pancreatic cancer, but PanCAN does not recommend nor endorse any particular health care resource. In addition, please note that any personal information you provide to PanCAN’s associates during telephone and/or email communications may be stored and used to help PanCAN achieve its mission of assisting patients with, and finding cures and treatments for, pancreatic cancer. Stored constituent information may be used to inform PanCAN programs and activities. Information also may be provided in aggregate or limited formats to third parties to guide future pancreatic cancer research and treatment efforts. PanCAN will not provide personal directly identifying information (such as your name or contact information) to such third parties without your prior written consent unless required or permitted by law to do so.